
Latest News

The CranioCradle – A Therapy Gadget Worth Getting?
We’re not usually huge fans of therapy gadgets as they tend to be a bit faddy and then they end up chucked at the back of the cupboard, however, our clinic manager, Fiona, has been trying out the CranioCradle. This claims to help promote relaxation and to even send you off to dozyland and can […]

Safety Concerns Regarding CrossFit
CrossFit is a fitness or lifestyle program that is gaining popularity in the UK. It works on the basis of setting a different fitness challenge each day to test various aspects of fitness. As with every sport or activity, injury can happen, particularly when participants are following a program online or in a large group […]

Misconceptions About Lactic Acid (or Lactate)
We all know that feeling after a hard workout or if we haven’t done any exercise for a while where the muscles become tight and really sore. There’s an endless supply of information that would tell you that this feeling is caused by the build up of lactic acid in the muscles, hence most people believe […]

Working As a Student at Elite Therapy
A few months ago, we introduced our new student, John Balshaw to you. You’ll meet John at the clinic usually on Tuesdays and sometimes later in the week too and he’s very much part of our team now! For any aspiring Sports Therapists out there, John has given this great insight as to what his […]

Warming Up in The Cold
We’re looking at ways you can stay active without getting wet and cold but what about if you don’t have much choice or if you’re one of those who doesn’t mind exercising in the wet and cold? Well, the best piece of advice we can give you to stay injury free is to warm up […]

How to Dress for Winter Activity
We now have a wonderful array of clothing choices available to us to allow us to train with comfort in the winter months and keep warm without losing movement and without having a major melt down! However, knowing how to put what layer where, how many layers and what materials can be a minefield but […]

Feet First – A Quick Guide to Flat Feet (Fallen Arches)
Feet are often overlooked and somewhat taken for granted in our daily lives until they start causing pain. One cause of pain may be so called ‘flat feet’ or fallen arches which sometimes can be painful, though sometimes not! John Balshaw offers some advice if you think you have flat feet: Flat feet, fallen arches […]
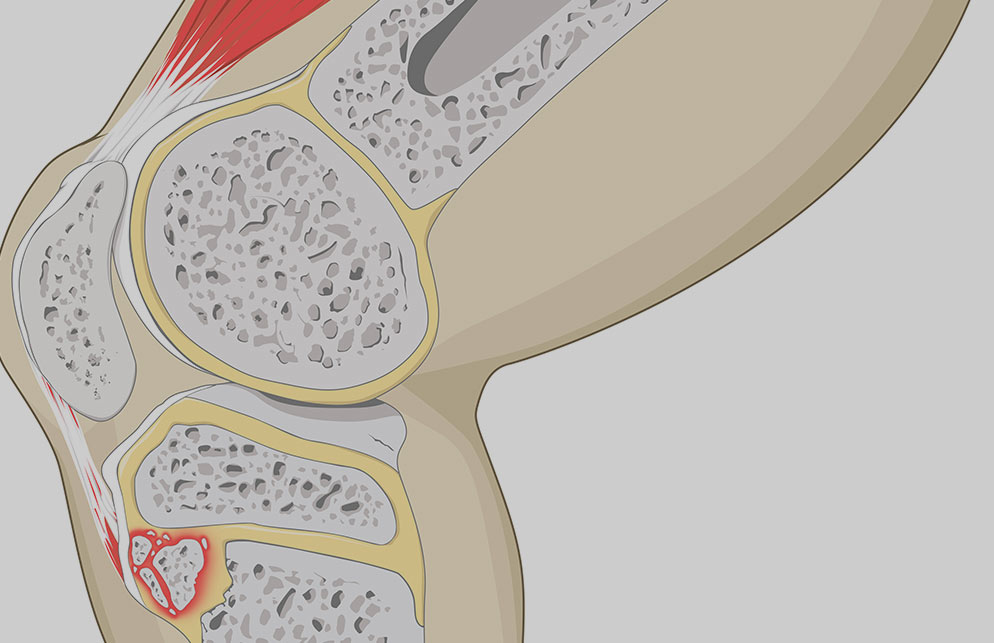
Osgood Schlatters Disease – What You Need to Know
If you have a child that’s diagnosed with Osgood Schlatters Disease, do you know what it is, what causes it and what you should do about it? Our Coventry Uni Sports Therapy student, John Balshaw explains the facts that you need to know: Osgood Schlatters Disease affects mostly teenage/adolescent children, more commonly boys and is […]

Anyone for Cricket? Fitness and Common Injuries In Cricketers
The game of cricket has changed so much in the past twenty years, with the introduction of One Day and Twenty20 as well as test matches, the game has never been so popular. It was once considered a game where fitness was never really that important, technical skills were enough, however, the Aussies soon changed […]

When Bigger Is Not Better – The Health Issues Associated With Big Breasts
We all, whether we like it or not, live in an age where the image of the human form, both male and female, is greatly distorted and there is great pressure to have a ‘perfect’ body, whatever that means or is. Is it fair to say that this pressure has been prevalent for females for […]

The Menopause and How Physiotherapy Can Help
There’s been a great deal of coverage in the press recently about the menopause to help raise awareness of what women may be experiencing during this phase of their life. The BBC ran a whole series of daily features on the subject to help raise understanding of partners, family members and employers about the symptoms […]

The Pushing, Pulling and Shoving of Daily Life – Look After Your Core
For so many of us, we take movement for-granted, we don’t think too much about lifting, pushing, pulling in whatever it is we’re doing, be it at home or in the workplace. But how often do we see someone in the clinic with bad back or neck pain that occured after doing something really simple […]

Housework and Gardening – Avoiding Injuries!
Extreme Spring Cleaning Injuries Explained… Extreme spring cleaning…? What am I on about and why am I writing about it? Well, it’s that time of year isn’t it? A bit of nice weather (and it was only a bit) but it’s enough to get us top to toeing the house, chucking stuff out, sorting out […]

A Quick Guide to Neck Pain
We’re seeing a lot of stiff and sore necks at the moment so lets take a quick look at causes and what can be done to help… Constant use of smartphones and tablets and ‘mobile’ technology also has an impact on posture and pain. Put it down! A painful neck can be anything from sore […]

